Main Navigation
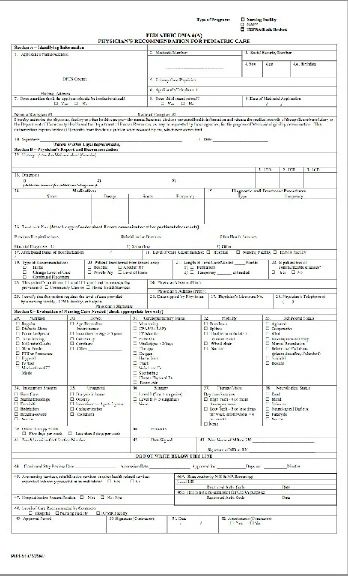
DMA6 Form for Medicaid
blank and filled in DMA 6 forms (with attachments) for the Katie Beckett Medicaid Waiver DMA 6 Form Filled In
double click image for larger document
for items #12, #13, #14 & #16 attachments
click here
DMA 6 Attachment for Items 12, 13, 14 and 16
Eliana Rachael Fier DOB 10/25/2002
Item 12. History and the Previous Hospitalizations portion of Item 16.
Eliana was born at 40 weeks gestation. She weighed 7lbs, 8 oz. Hypotonia was diagnosed at 9 months. At 10 months she was diagnosed a severe gross motor delay. PT was started 2X/week. Regression of developmental milestones began. An OT evaluation at 12 months found her to be at <1%ile for her age for gross and fine motor development. OT 2X/week and Speech therapy 1X/week were started at 13 months.
On 11/16/03 – 11/20/03, at 12 ½ months, she was admitted to the Egleston Intensive Care Unit with a diagnosis of Status Asthmaticus. She required oxygen, IV steroids, and racemic epinephrine to stabilize her. She was readmitted 9 days later (ER 11/29/03, inpatient 11/30/03-12/10/03) with similar symptoms. A work-up of her developmental delay was initiated. On 12/3/03, a swallow study showed aspiration of thin and thick liquids; an NG tube was placed and tube feedings were started. On 12/3/03, an abdominal ultrasound showed a slightly enlarged liver. On 12/4/03, an ophthalmologic exam revealed a cherry red spot diagnostic of a lysosomal storage disease. On 12/5/03, enzyme studies confirmed a diagnosis of Tay-Sachs disease. On 12/5/03, a brain MRI with SPECT showed mild cerebellar and cortical atrophy. On 12/9/03, a PEG tube was placed. On 12/10/03, she was discharged home.
From the ages of 12 months to 24 months, Eliana experienced regression of milestones until she was assessed as being at the developmental age of “less than one month.” She was blind by 18 months. She was essentially paralyzed with little to no control of her arms and legs. She still had some head and neck control and she was able to prop sit with support. Seizures began during this period and worsened over time. GI motility was an ongoing problem with severe constipation, gastric distention, reflux, and aspiration of stomach contents. Reglan, Prilosec, and Miralax helped, as did the use of Peptamen Junior for nutrition. Her breathing became weaker and she took Xopenex nebulizer treatments every 6 to 8 hours around the clock, Pulmicort treatments once a day, Atrovent as needed, and Singulair by G-Tube at night. She was prescribed the Vest for chest physical therapy and used it twice a day for 20 minute sessions. She also required a lot of manual chest physical therapy and suctioning as needed around the clock.
On November 17, 2004, at the age of two, Eliana was admitted to Egelston Hospital for 10 days. She had a GI Bleed, possibly related to an extended course of prednisone earlier that month. She was also found to have dilated loops of bowel, a partial ileus, and a high fever. She was admitted and continued to have temperature spikes. She vomited and aspirated her stomach contents the next day and was admitted to the ICU in respiratory distress. She was given CPAP with her nebulizer treatments, a cooling blanket, IV fluids, peripheral nutrition, and other supportive care. Temperature spikes continued even after IV antibiotics were started. Blood and urine cultures were negative. Bloodwork was negative. Chest X-rays showed a new pneumonia. After 4-5 days, a second IV antibiotic (Cleocin) was started, with normalizing of temperature and improvement of respiratory status. During her stay, General Surgery followed her for her partial ileus and decompressed her bowels twice using a rectal tube. She was transferred to a general floor for 4 more days. She required a PIC line for TPN after her 5th day with only peripheral nutrition; this was taken out before discharge. She resumed Peptamen feeds without difficulty. Prilosec was changed to Prevacid. All other medications stayed the same. She was discharged on November 27, 2004. Her IV Cleocin was changed to oral Cleocin, which she took for 5 more days.
From the age of two to three, Eliana regressed further. She had frequent reactive airway episodes (likely due to aspiration), typically requiring a short course of prednisone, an increase in frequency of nebulizer treatments up to every 1-2 hours, frequent suctioning throughout the day and night, and frequent CPT. She also required antibiotics (Amoxicillin, Keflex, Clindamycin) a number of times. Nebulized Pulmicort was increased to twice a day. Reglan and Miralax doses were increased to help improve gastric motility and decrease reflux. Tube feeds were slowed down from 180 cc/hour to 100 cc/hour. Constipation was severe and enemas were used when constipation resulted in excessive gastric distention. Bowel functioning was monitored carefully due to its negative impact on reflux, respiratory functioning, and aspiration risk. In August 2005, Zavesca, a substrate inhibitor, was started as a treatment for Tay-Sachs disease. It caused gastric distress for the first 6 to 8 weeks of treatment.
In October 2005, at the age of three, Eliana aspirated her stomach contents and suffered from a severe bout of aspiration pneumonia. She was treated at home, but with an ICU level of care, with 24 hour intensive nursing/medical care. She received nebulizer treatments every 1-2 hours, oxygen around the clock, and aggressive Chest PT. She required frequent suctioning. She was febrile and required a course of Clindamycin.
Approximately 6 weeks after completing the course of Clindamycin, she started having GI bleeding and appeared to have colitis due to the antibiotic. Her stools tested positive for occult blood, but her hemoglobin and hematocrit remained stable. Yogurt was started as a pro-biotic agent, and the bleeding stopped. She continues to take yogurt 4 times a day in all of her G-tube feedings.
From the age of three to six, Eliana followed the typical course for Tay-Sachs disease, which will be broken down by system:
Neurologic: Eliana started having myoclonic seizures in March 2004, from 5-20 a day. She also had choreoathetosis, hypertonicity, clonus, muscle rigidity, and an exaggerated startle reflex. Diastat per rectum was prescribed for prolonged seizure activity. Benadryl was started to try to decrease muscle rigidity, spasticity, and choreoform movements. Klonopin was started for muscle relaxation and seizure control. Klonopin was very effective. Eliana continued to have seizures over the years and her dose of Klonopin has slowly increased. (Her dose was just recently increased to 1mg 4X/day or a total of 4mg/d). In June of 2007, a second anticonvulsant, Lamictal, was started; it was slowly increased over the years to its current dose of 100 mg at 12pm and 75mg at 12am. Eliana continues to have seizures many times a day. Her seizures include eye roving, stiffening or rigidity of parts or all of her body, typically followed by a complete loss of tone. In some positions, the seizures cause her to turn blue, however this can be corrected with repositioning of her body and head. If the rigidity is in her trunk during or after a feed, the seizure may induce vomiting. Again, repositioning often helps. She has required Diastat per rectum a few times over the years. Eliana is constantly monitored for seizure activity and the resultant asphyxiation or vomiting the seizure may cause. In more recent months, she has had apneic episodes during rather quiet seizure activity. It is for this reason that her Lamictal and Klonopin doses have been titrated up.
Muscular: Eliana requires frequent repositioning of her extremities and her head due to spasticity, clonus, hyperextension, and exaggerated startle responses. She requires ankle-foot orthotics due to ankle contractures. In the fall of 2006, she had hip-knee-ankle-foot orthotics made, which has allowed for standing. Since she turned four, stiffening at the hip and thighs has increased, making diaper changes and hygiene difficult. In addition, ankle and wrist contractures formed and worsened. In the spring of 2007, she was fitted for wrist splints due to wrist contractures. New AFOs were made to because her ankle could no longer be place at a 90 or 120 degree angle without causing pressure points and skin breakdown. Baclofen was started in an attempt to decrease muscle tone, and she is currently taking 10mg a day. In June 2007, she was evaluated by and Orthopedic surgeon and was found to have hip dislocation and ankle contractures which would benefit from tendon release surgery. Because she cannot safely undergo anesthesia, the surgery was not done. Botox injections were strongly considered, but have not yet been tried. After Lamictal was started in June 2007, and Klonopin was increased slightly, her stiffness improved slightly. Eliana has a physical therapy routine which is done each day as tolerated.
GI: As detailed above, Eliana is treated for GERD, poor gastric motility, severe constipation, and gastric distention. She has had GI bleeds and a partial ileus. She requires close monitoring of bowel functioning because the gastric distention caused by constipation can cause regurgitation of food and possibly aspiration into the lungs. It also results in a decrease in lung capacity and functioning. It has also been noted that seizure activity worsens when she has abdominal distention and discomfort. Her constipation is treated aggressively with daily Miralax, an elemental formula, a promotility agent, exercise, and water. She has required rectal stimulation up to 2-3 times per week when bowel functioning is slowed.
Pulmonary: Eliana has chronic lung disease and has required around the clock nebulizer treatments for the past six years. Every three hours she receives Xopenex alone, or in combination with Atrovent or Pulmicorte. She uses the Vest for chest physical therapy twice a day, and she uses a Cough Assist machine every six hours before feedings. A scopolamine patch helps to control oral secretions. She is suctioned throughout the day. Eliana requires oxygen via nasal cannula whenever she spikes a fever, and she has an oxygen concentrator at home. She has had a number of pneumonias over the years requiring the use of antibiotics and steroids. Eliana chokes on her secretions and must have a caregiver by her side at all times. Eliana was oxygen dependent from the end of February to the beginning of March 2011. She required a course of prelone and Azithromycin for a possible pneumonia.
Cardiac: Eliana’s heart rate is normally between 100 and 125 beats per minute. When she is febrile, her heart rate increases to over 150 beats per minute. Over the 2-3 years, temperature disregulation has been severe. Her temperature will rise above 105 degrees when in the sun (this was tolerated very well in the past), and will dip down to 92 degrees (axillary) if not covered up appropriately. When cold, her heart rate will drop to 60-80 beats per minute. Her caregivers monitor her body temperature every 1-3 hours and adjust the room temperature accordingly.
Endocrine: Eliana has Precocious Puberty, which started with breast buds at the age of four. She now has axillary and pubic hair as well as vaginal discharge. She was evaluated by an endocrinologist in December 2007. Lab tests confirmed this diagnosis, which is likely due to seizure activity near or on the pituitary gland. Her family has opted against treatment with monthly Lupron injections. In May 2010, she had symptoms of PMS and had a small, red discharge assumed to be a menstrual cycle. She had similar episodes in August of 2010 and January 2011. As noted above, she has severe body temperature dysregulation and must be monitored closely for extremes in body temperature; she can fluctuate from 92 to 103 degrees depending on how hot or cold her immediate environment is.
Urologic: Eliana sometimes retains urine for 8 to 12 hours, though she typically urinates at normal intervals. She has not had any UTI’s and has not required catheterizations. This is monitored closely. Bladder massaging has been effective. During her PMS episodes, her abdominal distention helps her to urinate on her own.
Infectious disease: Eliana has had ear infections, strep throat, sinus infections, and pneumonia over the years. She is susceptible to normal childhood infections. She received the combined flu vaccinations this year. She recently completed a course of Azithromycin for a suspected pneumonia.
Skin/Mucus Membranes: She is monitored closely for skin breakdown. AFO’s are worn for only 2 hours at a time due to her history of skin breakdown and ulcers forming where the AFO’s rub her heal. Eliana has regularly seen an ophthalmologist since July 2009, every week for a while. She has a corneal abrasion that has not healed. She had her eye-lid sewn partially shut on October 27, 2009 to improve healing. Her left eye remains partially closed and looks clear and perfectly healed. Since 2010, her right eye developed an opacity which has persisted despite eye drops around the clock and eye lubricant every 3 hours. She will see the eye doctor on 3/17/11 to assess the need for surgery on her right eye.
Item 13: Diagnoses
1) Tay-Sachs disease 2) Seizure Disorder 3) Chronic Lung Disease 4) Blindness 5) Severe Developmental Regression/ Paralysis 6) H/O Aspiration Pneumonia 7) PEG-feeding dependent 8) Swallowing Dysfunction 9) GERD 10) Reactive Airway 11) Severe Constipation 12) S/P GI Bleed 13) Delayed Gastric Motility 14) Urinary Retention 15) Hip, Ankle and Wrist Contractures 16) Corneal Abrasion 17) Precocious Puberty
Item 14: Medications
Pulmicort Nebs 0.25 mg 2X/d Prevacid 15 mg 2X/day
Klonopin 1.0 mg 4X/d Miralax 17 mg a day + PRN
Xopenex Nebs 0.63 mg Q3HRS and PRN Atrovent Nebs 0.25 mg 2X/day & PRN
Zavesca 100 mg 3X a day Scopolamine Transdermal Patch 1.5 mg Q 48 Hrs
Polyvisol with Iron 1cc QAM Peptamen Jr. 5 ounces 4X/day
Diastat 10mg PRN for seizures Lamictal 100 mg at 12 pm and 75mg at 12 am
Reglan 2mg 4X/day Baclofen 10mg/day
Singulair 4 mg each night Maalox 5cc 1X/day & PRN
Benadryl 7.5mg 4 times a day Lacrilube to eyes 3X/d
Artificial Tears to both eyes every hour Completed a course of Prelone & Azithromycin 300mg/day on 3/5/11
Item 16: Treatment Plan
Previous Hospitalizations and admitting diagnoses are listed above under Item 12.
A detailed treatment plan can be found in the document, “CARE PLAN: March 2011”